A Role for VSIG-3/VISTA Signaling in Acquired Resistance to Anti-PD-1 Therapy?
Immunotherapy has revolutionized the way we treat cancer. Ground breaking studies have demonstrated that co-signaling molecules such as cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), programmed cell death 1 (PD-1) receptor, and programmed death ligand 1 (PD-L1) are an important therapeutic targets. However, these victories have been tempered by the development of acquired resistance in some cases. Why is this happening? What are the mechanisms of acquired resistance to immune checkpoint blockade?
VSIG-3 is a novel ligand for VISTA
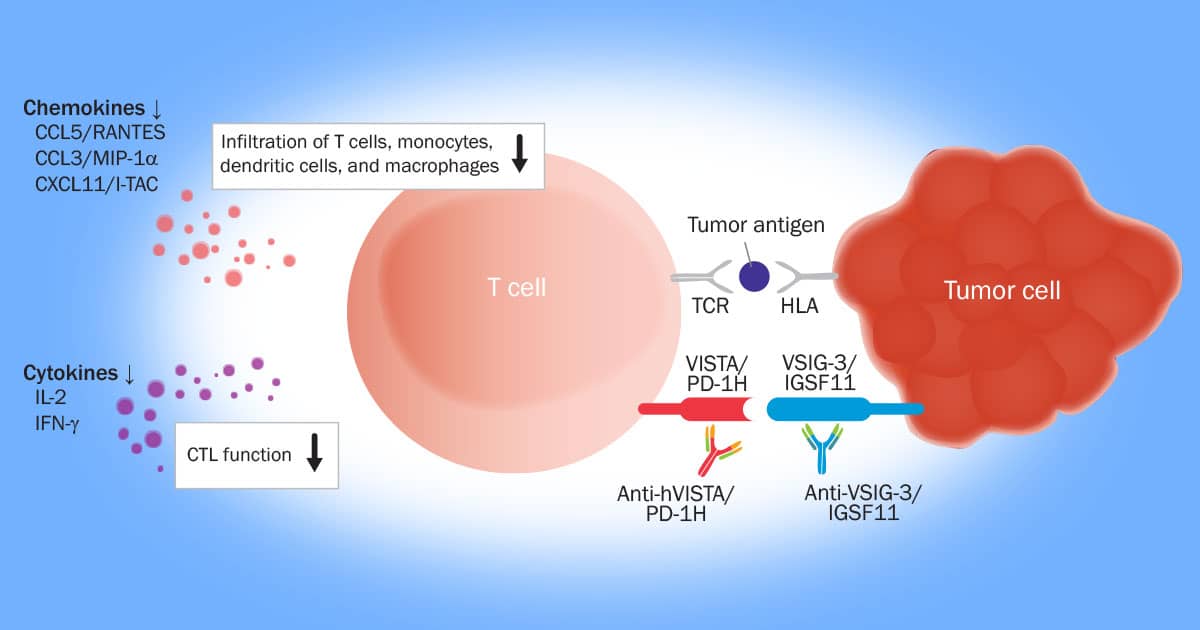
Recent work from R&D Systems scientists has shown that V-Set and Immunoglobulin domain containing 3 (VSIG-3), is a novel ligand of the V domain-containing Ig suppressor of T cell activation (VISTA). VISTA is expressed on a number of immune cell types including: CD11bhigh myeloid derived APC’s, CD4+ T cells, CD8+ T cells and Tregs. VISTA has been shown to be a co-inhibitory receptor on CD4+ T and a co-inhibitory ligand for T cells. Using a functional ELISA Assay, R&D Systems scientists first demonstrated that recombinant VSIG-3 binds to recombinant VISTA. VSIG-3 was subsequently shown to inhibit chemokine and cytokine production in peripheral blood mononuclear cells (PBMCs). The specificity of the VSIG-3/VISTA interaction was verified by the observation that recombinant VISTA attenuated VSIG-3 mediated inhibition of CCL5/Rantes and IL-17 in anti-CD3 activated PBMCs. Finally, VSIG-3 was shown to negatively regulate human CD3+ T Cell activation, indicating that VISTA and VSIG-3 are part of a co-inhibitory pathway that inhibits T cell activation.
Negative Immune Checkpoint Regulation by VISTA May Be a Mechanism of Acquired Resistance to anti-PD-1 Therapy in Metastatic Melanoma
Although acquired resistance is a common response to anti-PD-1 immunotherapy, less is known about the mechanism underlying it. Kakavand et al., investigated potential mechanisms of acquired resistance in biopsies from metastatic melanoma patients that showed cancer progression after initially responding to PD-1 and/or CTLA-4 immunotherapy. Biopsies from patients prior to immunotherapy were matched with biopsies taken from the same patients that showed post immunotherapy cancer progression. Using immunohistochemistry, Kakavand et al., observed, among other things, an increased number of VISTA+ intratumoral lymphocytes. In their discussion, Kakavand et al., made 2 relevant observations. 1. “The frequent observation of increased expression of intratumoral VISTA+ lymphocytes during acquired resistance to immune checkpoint inhibitor therapy suggests that this is probably an important mechanism of resistance”. 2. “The binding partner to VISTA has not yet been identified”.
A Role for VSIG3 in Acquired Resistance to Anti-PD-1 Therapy in Metastatic Melanoma?
How does this all tie together? Quite simply, the accumulating evidence suggests that the VISTA/VSIG-3 co-inhibitory pathway represents a potential therapeutic target for overcoming acquired resistance to PD-1 checkpoint inhibition in metastatic melanoma! More research is needed to assess the relationship between VISTA/VSIG-3 signaling and acquired resistance to immunotherapy.